
General info

With a comprehensive knowledge of the latest materials and techniques, the prosthodontist is spoiled for choice when considering different treatment options for the restoration of decayed or worn teeth and the replacement of missing teeth. Dental implants, fixed partial dentures (bridges) or removable dentures can all be successfully utilised in replacing missing teeth whereas the rehabilitation of compromised teeth can be done with a variety of techniques which include ceramic inlays/onlays, crowns and veneers, or state-of-the-art composite resin materials.
The health of the supporting structures such as the tooth root and surrounding bone is just as important. Prosthodontists are trained to deliver advanced root canal treatment to revive some of the most compromised teeth.
The healthy function and maintenance of oral tissues exists within the harmonious interaction between the neuromuscular control of the muscles of mastication and the relationship of the teeth with the former. Occlusal/ bite discrepancies can be involved in jaw joint and muscle problems and the correction/ management of these imbalances can be dealt with by a prosthodontist.
Dental implants

A dental implant is a titanium “screw” device used in dentistry to replace the root structure of a missing tooth. This new titanium “root” is fitted with and support a restoration/s that resemble a natural tooth or group of teeth in need of replacement.
Dental implants have revolutionized prosthodontics and can be used to support a number of dental prostheses, including crowns, implant-supported bridges or dentures. Dental implants have become the standard of care for the replacement of teeth because they allow a missing tooth (or teeth) to be restored without invading or damaging any other teeth or tissues. It is therefore the perfect alternative to a conventional “bridge” where the teeth on either side of the space are prepared for crowns and a false tooth suspended between them.
Dental implants can also replace multiple missing teeth which are traditionally replaced by a removable partial denture. They can be used as anchors for a fixed bridge to replace the teeth making the removable partial denture obsolete. In some cases, there are too many teeth missing to use a fixed bridge; however, using a dental implant with an attachment that snaps into the removable partial denture will significantly improve its stability and improve the patient’s chewing function and confidence. Perhaps the best-known use of dental implants is treating patients without any teeth. Denture wearers often suffer from loose and “floating” dentures, and dental implants offer many benefits to patients without teeth. Stability of the dentures is improved with the use of even one or two dental implant/s with attachments, but greater satisfaction is achieved as the number of dental implants is increased. Depending on the number of implants utilized a denture can be made that clips onto a bar supported by the dental implants or a fixed denture that is permanently attached to the dental implants. An added benefit of implants is the preservation of the patient’s jawbone as it retard the shrinking of the jaw that is routinely seen in long-term denture wearers. Talk to a prosthodontist today about using dental implants to increase your confidence and quality of life.
Crowns and Bridges

Restorations that fall under this category of treatment options include inlays, onlays, veneers, crowns, and bridges (fixed partial dentures). These restorations are fabricated by highly skilled dental technicians using state-of-the-art technology to produce bio-mimetic and life-like replacement parts for lost teeth or tooth structure. They can be constructed from a variety of materials, e.g., porcelain, ceramic, composite resin, and metal, of which the prosthodontist will decide which to use for a given situation.
The use of these restorations is mainly indicated when a tooth has a cavity that is too large to restore with a conventional restoration/filling. Veneers and crowns can also restore or improve dental aesthetics, often with startling results.
Prosthodontists undergo extensive training to enable them to appropriately prepare teeth and take impressions to ensure fabrication of restorations that approach a perfect fit to the tooth. This is a critical requirement, as the life expectancy of the tooth and restoration is closely related to this factor.
Sometimes the restorative challenges are very large, involving the restoration of many, or even all teeth, and this will test the skill of even a specialist.
Tooth whitening
When it comes to tooth whitening, every patient is different. Patients have different lifestyles and smiles with varying needs, which means it is unlikely a single whitening product is a “one size fits all”.
That is why it is important to offer my patients a choice – and with NOVON® White Dental Beauty’s professional tooth whitening systems I can do just that.
How does it work?
White Dental Beauty tooth whitening gels have a variety of different strengths, all powered by NOVON® – a whitening compound that delivers improved whitening results over less treatment time.
NOVON® has a unique inherent feature in that, on application, it produces a “pH jump” into the alkaline pH range.
This “pH jump” enhances the release of perhydroxyl ions for a faster whitening effect. NOVON® containing gels can therefore produce a similar whitening effect within a shorter time frame, in comparison to regular whitening gels.
What if I have sensitive teeth?
Up until now, people with sensitive teeth have struggled to whiten their teeth or have had to avoid whitening all together.
White Dental Beauty Mild is a gentle and safe tooth whitening gel that has been formulated to help reduce sensitivity when whitening your teeth. The unique 5% CP formula of White Beauty Mild enables the same results as a standard 10% CP gel, but with overall less sensitivity.
Endodontic treatment

Tooth decay, trauma (e.g., tooth fracture), periodontal disease, restorative procedures, and a variety of other pathological processes can have a direct impact on the nerve and blood supply of the tooth (pulp). Injury to the pulp may present with a range of clinical signs and symptoms that might take the form of dental hypersensitivity (e.g., thermal hypersensitivity), pulpitis (acute/chronic tooth ache), and in severe cases, pulp necrosis (a loss in tooth vitality), with the development of a dental abscess.
Prosthodontists receive in depth training in the diagnosis and treatment of injury to the pulp that range from pulp maintenance procedures (dressings on exposed pulp) to the removal of the pulp (root canal treatment).
It is important that root canal treatment is done to very high standards to cure abscesses. You can only treat what you can see and as part of his armamentarium the prosthodontist makes use of exceptional high quality equipment in the form of a micro CBCT (3D X-ray) for diagnostic purposes and a high resolution microscope for the accurate execution of treatment.
Temporomandibular joint disorder (TMJD)

The lower jaw articulates with the base of the skull via the temporomandibular joints (TMJs). The two joints are unique in a sense that they can both rotate and slide in all directions, making them vulnerable to trauma and degenerative changes. The temporomandibular joint is susceptible to many of the conditions that affect other joints in the body, including arthritis, trauma, dislocations, ankylosis, developmental anomalies, and neoplasia.
Temporomandibular disorders are therefore a collective term for pain and dysfunction of the masticatory muscles and TMJs.
Signs and symptoms
Signs and symptoms are often self-reported or provoked through self-palpation and/or movement of the jaw. They vary in their presentation and can be very complex, but are often simple.
Symptoms associated with TMJ disorders may be:
• Biting or chewing difficulty or discomfort
• Clicking, popping, or grating sound when opening or closing the mouth
• Dull, aching pain in the face (intermittent or persistent)
• Earache (particularly in the morning)
• Headache (particularly in the morning)
• Hearing loss
• Migraine (particularly in the morning)
• Jaw pain or tenderness of the jaw
• Reduced ability to open or close the mouth
• Tinnitus
• Neck and shoulder pain
TMJDs place a heavy burden on the patient, not only in the form of pain and physical debilitation, but also from a psychological and psychosocial point of view affecting daily living and quality of life!
Causes of TMD
There are many external factors that place excessive strain on the TMJ that can result in degenerative changes in the cartilaginous components of the joint.
These include but are not limited to the following:
• Bruxism (repetitive unconscious clenching or grinding of teeth, often at night).
• Trauma
• Malalignment of the occlusal surfaces of the teeth due to defective crowns or other restorative procedures.
• Jaw thrusting (causing unusual speech and chewing habits).
• Excessive gum chewing or nail biting.
• Degenerative joint disease, such as osteoarthritis or organic degeneration of the articular surfaces, recurrent fibrous and/or bony ankylosis, developmental abnormality, or pathologic lesions within the TMJ
• Myofascial pain dysfunction syndrome
Treatment
1. Restoration of the occlusal surfaces of the teeth
If the occlusal surfaces of the teeth or the supporting structures have been altered due to inappropriate dental treatment, periodontal disease, or trauma, the proper occlusion may need to be restored.
Patients with bridges, crowns, or onlays should be checked for bite discrepancies. These discrepancies, if present, may cause a person to make contact with posterior teeth during sideways chewing motions. These inappropriate contacts are called interferences, and if present, they can cause a patient to subconsciously avoid those motions, as they will provoke a painful response. The result can be excessive strain or even spasms of the chewing muscles.
2.Occlusal Splint
Occlusal splints (also called night guards or mouth guards) reduce nighttime clenching in some patients, while increasing clenching activity in other patients. Thus, while occlusal splints do prevent loss of tooth enamel from grinding, use of a splint can worsen TMJ disorder symptoms for some people.
3. Pain relief
While conventional analgesic pain killers such as paracetamol (acetaminophen) or NSAIDs provide initial relief for some sufferers, the pain is often more neurologic in nature, which often does not respond well to these drugs.
4. Jaw Exercises
Treatments for TMJ should not permanently alter the jaw or teeth but need to be reversible. To avoid permanent change, over the counter or prescription pain medications may be prescribed. Some sufferers may also benefit from gentle stretching or relaxation exercises for the jaw, which may be recommended by their healthcare providers.
5. Surgery
Exercise protocols, habit control, and splinting should be the first line of approach, leaving oral surgery as a last resort. Certainly, a focus on other possible causes of facial pain and jaw immobility and dysfunction should be the initial consideration of the examining oral-facial pain specialist, oral surgeon or health professional.
Maxillofacial prosthodontics
Maxillofacial prosthodontics is a specialty of dentistry which deals with the rehabilitation of patients with congenital or acquired defects of the orofacial region. Defects in this region can range from minor to major functional disabilities and cosmetic disfigurement that has a profound effect on the quality of life and psychosocial well-being of the individual.
Rehabilitation of orofacial defect can be very complex and almost always necessitates a multidisciplinary approach which involves various disciplines such as maxillofacial surgeons, plastic surgeons, radiologists, oncologists, head and neck surgeons, neurosurgeons, otolaryngologists, periodontists, orthodontists, social workers, speech therapists, and occupational therapists among others. The maxillofacial prosthodontist is often the orchestrator of the team as he/she should be involved from the start of treatment up until the end of the prosthetic rehabilitation and maintenance phase.
Birth defects
While craniofacial deformities such as cleft lip and palate are managed by various specialist doctors, the role of the maxillofacial prosthodontist is critical in supporting the surgical care in such patients when closures of openings between the oral and nasal cavities are achieved and should focus on providing supportive restorative structures to facilitate swallowing, chewing, and speech.
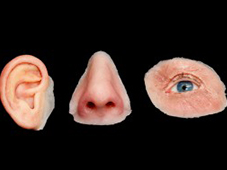
Cancer
The main objective in the management of malignant disease is cure, but there are important secondary goals to be considered as well. All effort is made in preserving form and function as to retain an acceptable quality of life for the patient. The advent of dental implants has vastly improved our ability to replace missing oral structures that are critical for the retention and restoration of teeth and other oral structures that restores chewing, swallowing and speech. Facial disfigurement can be overcome by restoration of eyes, ears, noses, or other facial structures, occasionally retained by cranial implants.
